|
Research Article
Diagnostic spectrum of non-neoplastic ovarian lesions in Nigerians: A seven-year hospital-based retrospective study
1 FMCPath, Lecturer, Department of Anatomic Pathology and Forensic Medicine, Nile University of Nigeria, Abuja, Nigeria
2 FMCPath, Consultant Pathologist, Department of Anatomic Pathology and Forensic Medicine, Asokoro District Hospital, Abuja, Nigeria
3 FMCPath, Associate Professor/Head of Department, Department of Anatomic Pathology and Forensic Medicine, Nile University of Nigeria, Abuja, Nigeria
4 FWACS (O&G), Associate Professor, Department of Obstetrics and Gynecology, Nile University of Nigeria, Abuja, Nigeria
5 FWACS (O&G), Senior Lecturer, Department of Obstetrics and Gynecology, Nile University of Nigeria, Abuja, Nigeria
6 FWACP (Lab Med), Consultant Pathologist, Department of Anatomic Pathology, Diagnostic Pathology Consult Ltd, Abuja, Nigeria
Address correspondence to:
Bamnan Collins Dallang
Department of Anatomic Pathology and Forensic Medicine, Nile University of Nigeria, Abuja,
Nigeria
Message to Corresponding Author
Article ID: 100041G06BD2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Dallang BC, Okwudire-Ejeh IA, Ezike KN, Mai AM, Asaolu OA, Kwari SD, Adeoye AO, Oguntebi EE. Diagnostic spectrum of non-neoplastic ovarian lesions in Nigerians: A seven-year hospital-based retrospective study. Edorium J Gynecol Obstet 2025;10(1):6–14.ABSTRACT
Aims: Ovarian lesions are an important cause of morbidity and mortality worldwide. They are classified as non-neoplastic, neoplastic, and inflammatory. Non-neoplastic lesions occur most frequently. This study aims to describe the diagnostic spectrum of non-neoplastic ovarian lesions in a Nigerian population and compare their frequency, diagnoses, and clinical presentations with other studies from Nigerian and other regions of the world.
Methods: This was a hospital-based retrospective descriptive study of histologically diagnosed non-neoplastic lesions of the ovary.
Results: About 42.8% (295/689) of the ovarian lesions that met the inclusion criteria were non-neoplastic. The age range of the patients was 15–70 years. The median age was 34 years. The 25–34 years age range, 41.0% (121/295), had the highest frequency, while the 55–64 years age range, 0.7% (2/295), was least. Common clinical features included abdominal pain, 81/295 (27.5%), menstrual abnormalities 74/295 (25.1%), and abdominal swelling 67/295 (22.7%). The diagnostic spectrum included cystic, solid, and inflammatory lesions. Corpus luteum cysts, 49.5% (146/295), were the most frequent, followed by follicular cysts, 28.1% (83/295). Polycystic ovary syndrome (PCOS), 0.7% (2/295), was the least encountered cystic lesion. Majority of the specimens, 41.0% (121/295), were small (<5 cm dimension), while the large (>15 cm), 13.9% (41/295), were least frequent.
Conclusion: Non-neoplastic ovarian lesions are an important cause of morbidity in the study population, with corpus luteum cyst as the commonest. Nulliparous and low parity patients were the most frequently affected. Timely and accurate histological recognition of these lesions are important for the purpose of institution of proper treatment.
Keywords: Corpus luteum cyst, Follicular cyst, Nigeria, Non-neoplastic, Ovary
INTRODUCTION
The ovaries are paired pelvic organs found on either side of the uterus [1]. Embryologically, they arise from both mesodermal (genital ridge) and endodermal (yolk sac) elements [2].
The clinically important ovarian lesions can be generally classified into non-neoplastic and neoplastic conditions [1],[3]. The non-neoplastic lesions predominate, and of these, the most commonly encountered are the non-neoplastic functional cysts [1],[3]. Non-neoplastic cystic lesions of the ovary include inclusion cysts, follicular cysts, cystic follicles, corpus luteum cysts, polycystic ovaries, developmental cysts, and epidermoid cysts [1],[3]. Other commonly encountered non-neoplastic lesions include luteomas of pregnancy, stromal hyperplasia, and hyperthecosis [1],[3].
Generally, the ovarian lesions show a broad spectrum of gross and histomorphological features. However, their clinical significance lies in their association with infertility and tendency to present as mass lesions hence mimicking neoplasms. They are also associated with menstrual abnormalities, and hormonal imbalances, including hirsutism and insulin resistance [4].
This study aims to describe the diagnostic spectrum of non-neoplastic ovarian lesions in a Nigerian population as seen in Asokoro District Hospital, Abuja, and compare their frequency distribution, lesion types, and clinical presentations with findings from other Nigerian studies and studies from other regions of the world. It is also hoped that this study, being the first of its kind to be carried out in this center, will help in the establishment of baseline data for health systems planning, especially in terms of infrastructural development, equipment prioritization, and resource deployment.
MATERIALS AND METHODS
Setting
Asokoro District Hospital (ADH) is located in Abuja, the capital city of Nigeria. The hospital is a tertiary referral center in Abuja and its Anatomic Pathology and Forensic Medicine Department receives an average of 2500 specimens annually.
Study Design
This was a hospital-based retrospective descriptive study of histologically diagnosed non-neoplastic lesions of the ovary. The study population included all cases with histologically diagnosed non-neoplastic lesions of the ovary at the histopathology department of ADH within the period of study (January 1, 2016 to December 31, 2022). Samples were obtained from ovarian cystectomies, oophorectomies, total abdominal hysterectomy and bilateral salpingo-oophorectomy specimens, and excision biopsies submitted to the ADH anatomic pathology and forensic medicine department from January 1, 2016 to December 31, 2022.
The patients’ demographic information and other clinical data were obtained from the departmental manual and hospital electronic records. Archival formalin fixed and paraffin embedded (FFPE) tissue blocks, and hematoxylin and eosin (H&E) stained slides of histologically diagnosed ovarian lesions were retrieved. Slides with poor or deteriorated quality were replaced by making fresh, 3 µm thick sections from the archival tissue blocks, and stained with H&E. All the slides thus obtained were subsequently reviewed by all four pathologists in the study to confirm by consensus, the diagnoses and other relevant morphological features.
Inclusion and Exclusion Criteria
Inclusion criteria
Cases with complete demographic data and those with adequately informative glass slides available were selected for the study. Cases where the slides were not found, but for which their FFPE tissue blocks were found, and therefore had new H&E slides produced were also selected.
Exclusion criteria
Cases with incomplete demographic data, and those where both glass slides and FFPE tissue blocks were not found, were excluded from the study. Cases for which there was no diagnostic consensus among the reviewing pathologists were also excluded.
Diagnostic Criteria
Gross specimen size was categorized according to their widest dimensions as follows:
- <5–9.9 cm = Medium
- 10–14.9 cm = Large
- ≥14.9 cm = Giant
Statistical Analysis
Data obtained were analyzed using analytical tools including Microsoft Excel software program (Microsoft Corporation, NY, USA) and analyzed with the Statistical Package for the Social Sciences (SPSS) Statistics for Windows, version 23.0 (SPSS Inc., Chicago, IL, USA). The data were presented in the form of tables and charts.
Ethical Consideration
Ethical clearance was obtained from the Medical Ethics Committee of Asokoro District Hospital via approval number: FCTA/HHSS/HMB/ADH/104/23.
RESULTS
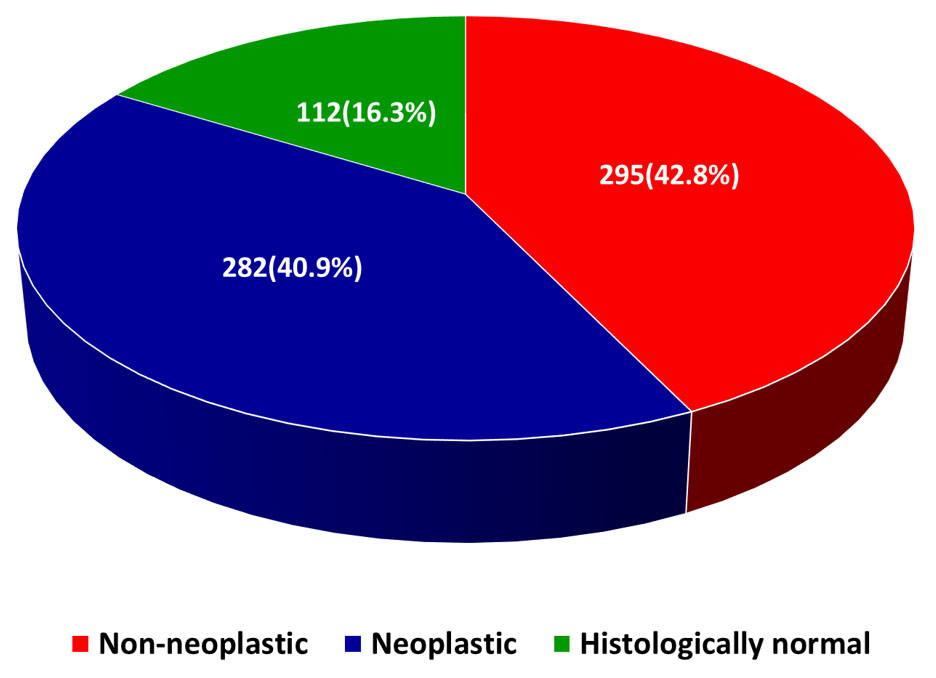
A total of 689 ovarian samples received within the study period met the inclusion criteria. Of these, 42.8% (295/689) were non-neoplastic lesions, while 40.9% (282/689) were neoplastic lesions (Figure 1).
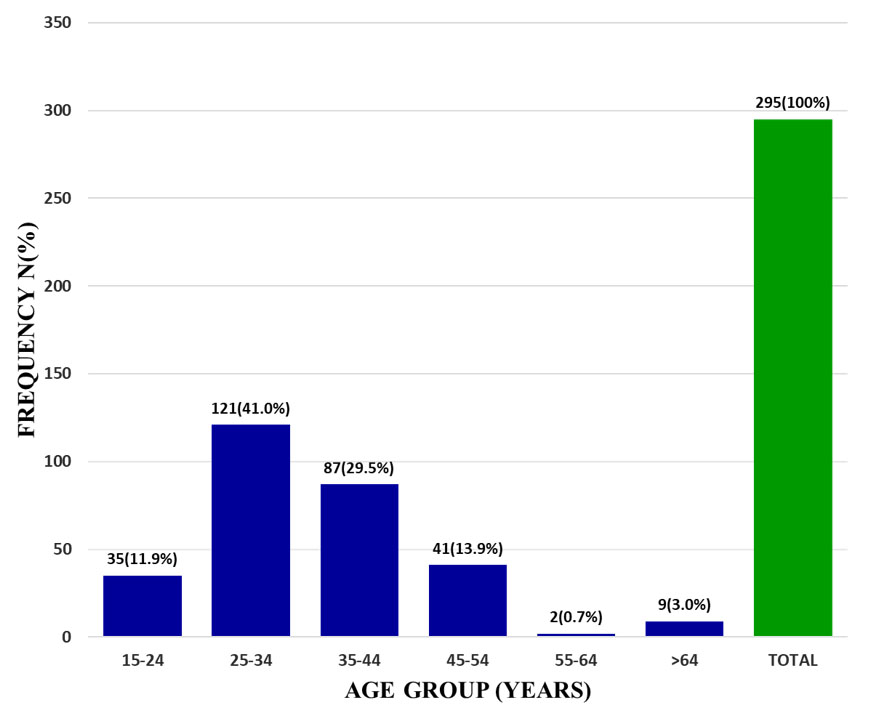
The age distribution of the non-neoplastic conditions showed an age range of 15–70 years. The mean age was 35.6±6.5 years while the median age was 34 years. The most frequent age group in which these lesions were diagnosed was the 25–34 years age group, who accounted for 41.0% (121/295), while the least was the 55–64 years age group with 0.7% (2/295) of cases (Figure 2).
Data on parity were available for 143/295 of cases. It showed that non-neoplastic lesions of the ovary were commoner in women who were either nulliparous 61/143 (42.7%) or of relatively low parity 55/143 (38.5%), as compared to women of parity greater than three 27/143 (18.9%).
The frequently encountered clinical features recorded include abdominal pain 81/295 (27.5%), menstrual abnormalities 74/295 (25.1%), and abdominal swelling 67/295 (22.7%).
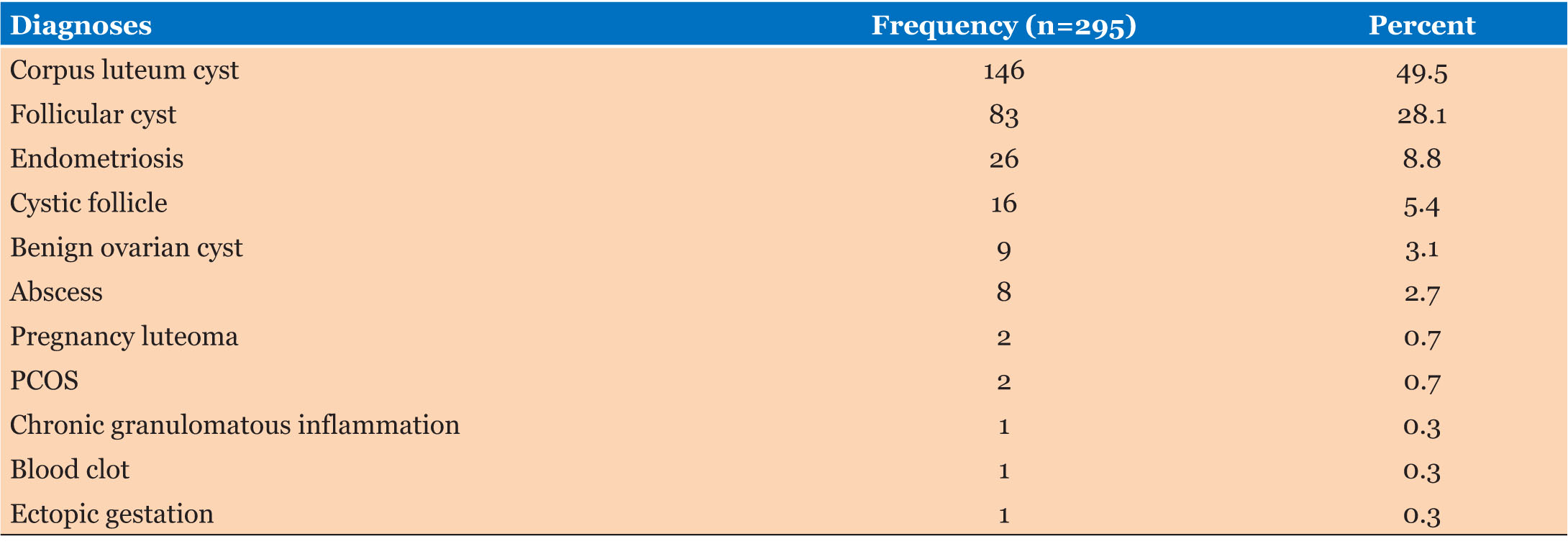
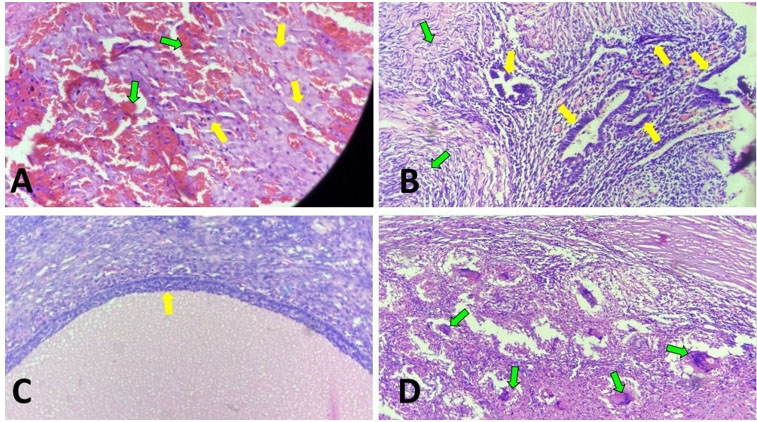
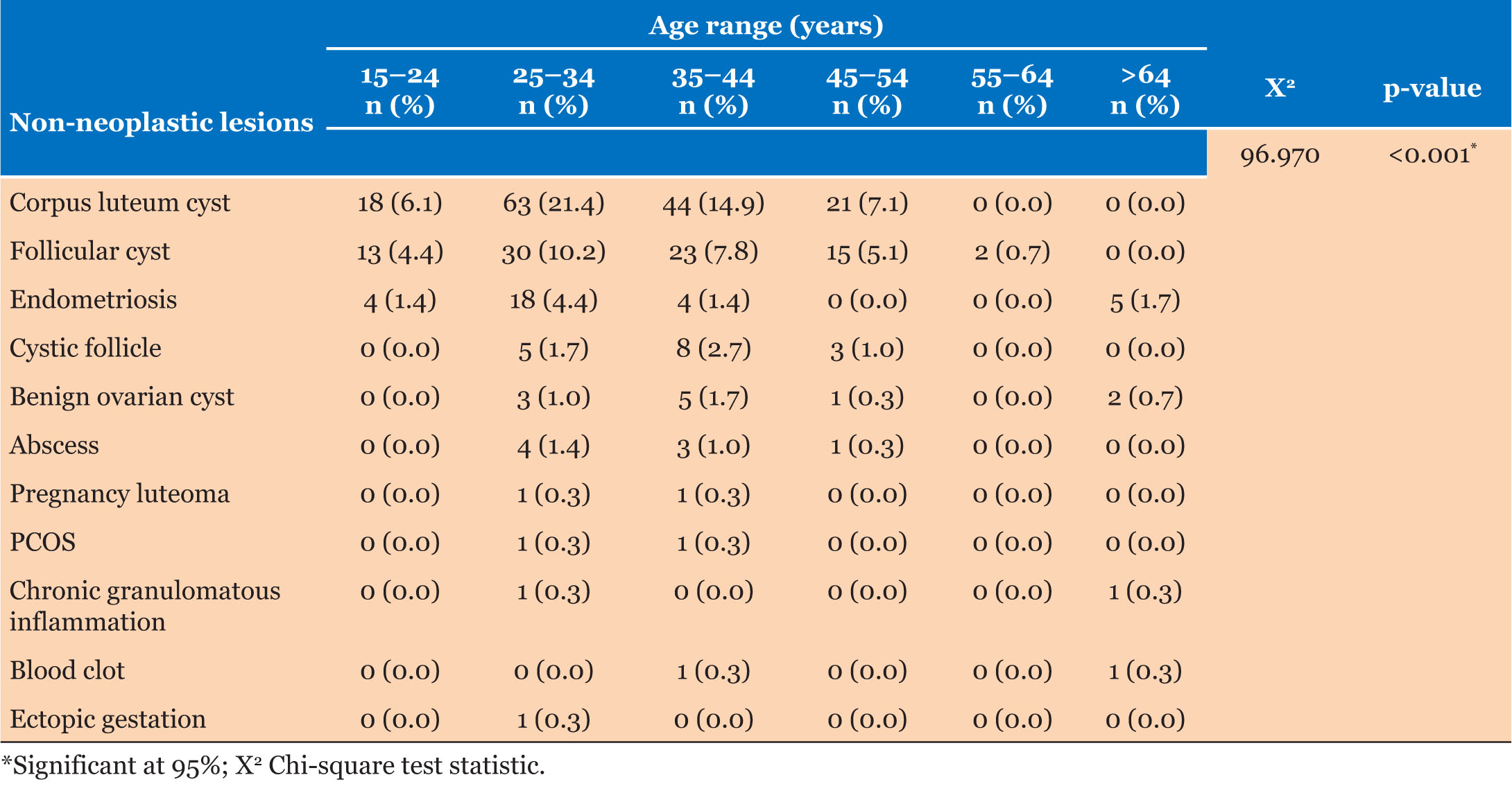
The diagnostic spectrum of the non-neoplastic lesions included cystic, solid, and inflammatory lesions. Corpus luteum cyst was the most frequently diagnosed, accounting for 49.5% (146/295) of cases, followed by follicular cyst, accounting for 28.1% (83/295). Polycystic ovary syndrome (PCOS) with 2 cases (0.7%) was the least encountered cystic lesion. Inflammatory conditions accounted for 3.1% (9/295) of diagnoses, and an overwhelming majority of these 88.9% (8/9) were ovarian abscesses; the only other diagnosis was a case of granulomatous inflammation in a 30-year-old patient (Table 1, Figure 3). The relationship between age and the various non-neoplastic disorders was statistically significant. A significant majority of corpus luteum cysts 85.6% (125/146) occurred in patients within the reproductive age range of 15–44 years. The age distribution of follicular cysts followed a similar pattern, occurring predominantly in the 15–44 years age range with a frequency of 79.5% (66/83) (Table 2).
Morphologically, majority, 55.5% (81/146), of the corpus luteum cysts were hemorrhagic but none of them was associated with torsion, while on the other hand, although only 8.4% (7/83) of follicular cysts were hemorrhagic, 4 out of the 7 (57.1%) were associated with torsion. A case of follicular cyst with hemorrhagic necrosis and degenerative osseous metaplasia was seen in a 21-year-old. All the endometriotic cysts seen were associated with increased fibrosis, hemorrhage, and presence hemosiderin laden macrophages.
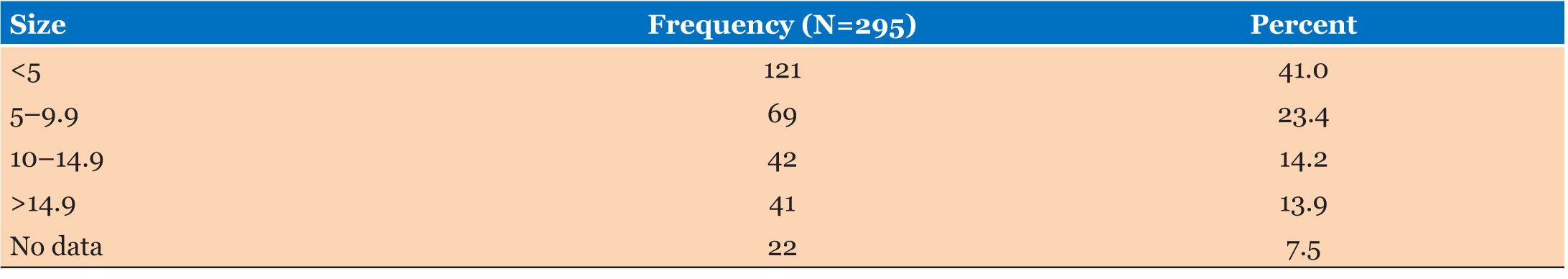
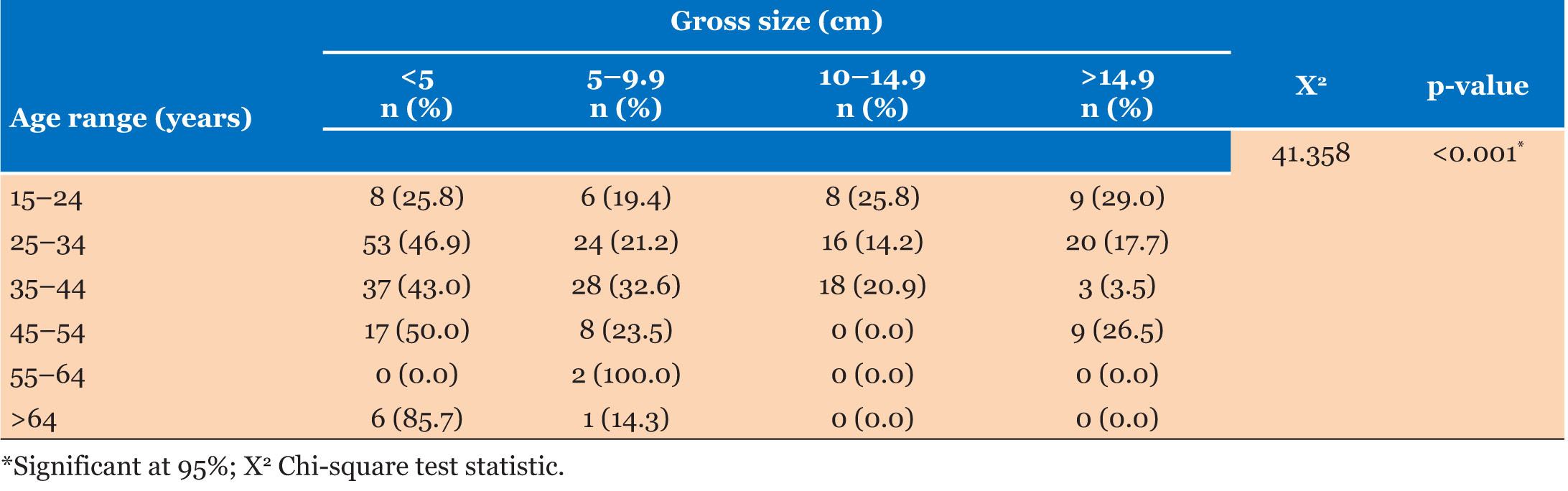
In terms of gross specimen size, small lesions (i.e., those that measured less than 5 cm in their greatest dimension) with 41.0% (121/295) of cases, predominated, while giant non-lesions (with largest dimension greater than 15 cm) were the least frequent with 13.9% (41/295) of cases (Table 3). The relationship between gross specimen size and the commonly encountered clinical features of abdominal pain, menstrual abnormalities, and abdominal swelling was not statistically significant. Of the 81 cases in which abdominal pain was encountered, the highest frequency of 34.6% (28/81) occurred in patients whose lesions measured less than 5 cm in greatest dimension. These findings were similar for menstrual abnormalities and abdominal swelling, with frequencies of 50.0% (37/74) and 29/67 (43.3%) for lesions measuring less than 5 cm in greatest dimension. In contrast, the relationship between gross specimen size and patients’ age was statistically significant. Patients in the early reproductive age range of 15–24 years had a preponderance of large and giant size lesions, 54.8% (17/31). In contrast, patients in the peri- and postmenopausal age ranges of 45 years and above had a much higher proportion, 79.1% (34/43), of small- and medium-sized lesions (Table 4).
DISCUSSION
Non-neoplastic lesions of the ovary constituted the majority of the ovarian samples obtained in this study, accounting for 42.8%. This is similar to trends obtainable in other parts of the world [1],[3],[5]. Some Nigerian studies carried out at Abuja and Benin also had similar findings [6],[7]. An Indian study by Gupta et al. which looked at ovarian masses in adolescents, as well as some other studies in the same region, also found non-neoplastic lesions to be the most frequent [5],[8],[9],[10],[11]. Functional cysts are known to be the commonest non-neoplastic lesions of the ovary [1],[3]. Consistent with this, we found corpus luteum cyst (49.5%) to be the commonest non-neoplastic lesion. Nigeria-based studies by Forae et al. and Innocent et al., in Benin and Jos respectively, also found corpus luteum cyst to be the commonest non-neoplastic lesion of the ovary [7],[12]. Follicular cyst was the second commonest non-neoplastic ovarian lesion seen in this study, accounting for 28.4% of these lesions. In contrast, an earlier study in Abuja, Nigeria, by Amin et al., found follicular cyst and corpus luteum cyst to be the most common and third commonest non-neoplastic lesions of the ovary respectively [6]. The reasons for this disparity are unclear but may be related to study methodology and differences in diagnostic criteria. Nevertheless, the etiology of these functional cysts being from physiological structures and processes, as well as their functional nature, underpins their common occurrence and their propensity for spontaneous resolution [1],[13],[14],[15]. They may however persist and attain significantly large sizes, enough to cause abdominal symptoms, or possibly rupture leading to life-threatening clinical conditions [13],[14],[15].
Even though non-neoplastic lesions of the ovary occurred over a wide age range of 15–70 years in this study, they were found to be most common in women in the 25–34 years age group and least common in post-menopausal women. This is similar to the age distribution seen in some studies around the world [7],[16]. The mean and median ages in this study (35.6±6.5 years and 34 years respectively) were similar to what was obtained in studies by Forae et al., Innocent et al., and Jones et al. [7],[12],[17]. This pattern of age distribution may be the result of greater exposure to physiological cyclical hormones in women that fall within the reproductive age group [1]. Further buttressing this, our finding that these lesions were commoner in nulliparous and low-parity patients underscores the contribution of hormonal exposure and uninterrupted menstrual cycles to the development of some of these lesions [1]. Other etiological factors include infertility treatment (with gonadotropins or other ovulation induction agents), tamoxifen, pregnancy, hypothyroidism, maternal gonadotropins, cigarette smoking, and tubal ligation [18],[19].
Similar to findings in other studies, a good number of our patients were asymptomatic, however, we also found abdominal pain to be a frequent clinical symptom [16],[18],[19]. The relationship between the size of a non-neoplastic ovarian lesion and its ability to elicit abdominal pain symptom is not straightforward, and depends on factors such as nature of the lesion, whether or not it is ruptured or infected or has undergone torsion and the patient’s pain threshold [16],[18]. For instance, patients with small endometriotic cysts often complain of cyclical pain while some may have follicular cysts that grow to relatively large sizes without experiencing abdominal pain [13],[20]. Perhaps, as a result of these factors, our study found no direct relationship between size and abdominal pain. Another clinical feature commonly encountered in this study; menstrual disturbances, also had no direct relationship with the size of the lesions. Menstrual abnormalities are a common feature of ovarian pathologies such as PCOS and pelvic inflammatory disease (PID) [21],[22]. Follicular cysts may be associated with endometrial hyperplasia and consequently, abnormal vaginal bleeding [13]. The likelihood of a non-neoplastic ovarian lesion causing abdominal swelling increases with the size of that lesion [23],[25]. However, our study did not demonstrate this relationship. The reasons for this are unclear but insufficient clinical details arising from lack of thoroughness in clerking and physical examination or laziness in entering these details in the electronic medical records by the clinician may be factors.
Our study found an inverse relationship between patients’ age and size of lesions, especially the cystic lesions. There is however no consensus on these as different studies report varying conclusions. Some, like Grigore et al., found no significant correlation between age and lesion size, while in keeping with our findings, Khan et al. reported an inverse relationship [25],[26]. One possible explanation is that these lesions occur more frequently in the reproductive years due to higher levels of hormone production by the ovaries in this age group [18]. Overall, most of the non-neoplastic ovarian lesions seen in this study were small, despite the common trend of small ovarian lesions being likely to resolve with conservative management and much less frequently requiring surgical intervention on account of large sizes [27],[28]. The differential diagnoses of these non-neoplastic ovarian lesions include other conditions, such as pelvic inflammatory disease, appendicitis, bowel obstruction, and rarer entities like gossypiboma, mesenteric cysts, or parasitic ovarian cysts, as all these conditions can present with non-specific symptoms like abdominal pain [24],[29].
Limitations of the Study
The major limitation of the study was that it was hospital-based and therefore analyzed only the cases that underwent surgical excision. As a result, the findings may not reflect the true prevalence and incidence of non-neoplastic lesions of the ovary within the population. Another limitation is the retrospective nature of the study design, which was associated with incomplete data, especially parity, with possible distortion of the rendered statistics. Inadequate storage facilities and retrieval of archival material also contributed to the inability to obtain some patient materials leading to exclusion from the study.
CONCLUSION
This study established that non-neoplastic ovarian lesions are an important cause of morbidity in the study population. It also demonstrated non-neoplastic lesions as the commonest conditions affecting the ovaries, and that corpus luteum cyst was the commonest of these lesions. These non-neoplastic lesions were found to be more common in women in the reproductive age group, especially nulliparous women and low parity women. Conversely, they were less common in post-menopausal and multiparous women. Their symptomatology was non-specific; hence, a high index of suspicion is required in the evaluation of these lesions. Aforementioned conditions, such as pelvic inflammatory disease, appendicitis, bowel obstruction, should also be considered in the differential diagnoses, along with rarer entities like gossypiboma, mesenteric cysts, or parasitic ovarian cysts, as all these conditions often present with similar non-specific symptoms like abdominal pain.. Their overlapping clinical features highlight the importance of thorough imaging and histological examination for accurate diagnosis and timely management.
REFERENCES
1.
2.
Atwi D, Ghofrani M, Hassell LA. Anatomy & histology. PathologyOutlines.com [Available at: https://www.pathologyoutlines.com/topic/ovarynontumornormalhistology.html]

3.
4.
Lengyel K, Hanley K. Polycystic ovary disease. PathologyOutlines.com [Available at: https://www.pathologyoutlines.com/topic/ovaryPCO.html]

5.
6.
Amin SM, Olah F, Babandi RM, Liman MI, Abubakar SJ. Histopathological analysis and clinical correlations of ovarian lesions in a tertiary hospital in Nigeria: A 10-year review. Ann Trop Pathol 2017;8(6):25–8. [CrossRef]

7.
Forae GD, Aligbe JU. A histopathological overview of ovarian lesions in Benin City, Nigeria: How common are the functional cysts? Int J Med Public Health 2014;4(3):265–8. [CrossRef]

8.
Gupta B, Guleria K, Suneja A, Vaid NB, Rajaram S, Wadhwa N. Adolescent ovarian masses: A retrospective analysis. J Obstet Gynaecol 2016;36(4):515–7. [CrossRef]
[Pubmed]

9.
Maurya G, Singh SK, Pandey P, Chaturvedi V. Pattern of neoplastic and non-neoplastic lesions of ovary: A five-year study in a tertiary care centre of rural india. Int J Res Med Sci 2018;6(7):2418–22. [CrossRef]

10.
11.
Hatwal D, Choudhari S, Batra N, Bhatt P, Bhatt S. Clinico-histopathological analysis of neoplastic and non-neoplastic lesion of ovary in Garhwal region of Uttarakhand: A 4-year study at tertiary level hospital. Indian Journal of Pathology and Oncology 2016;3(2):133–40. [CrossRef]

12.
Emmanuel I, Abobarin O, Abaniwo S, et al. A clinicopathological study of 236 cystic ovarian lesions at Jos University Teaching Hospital, Jos, Nigeria. Niger Med J 2022;62(6):360–4. [CrossRef]
[Pubmed]

13.
Turashvili G. Follicle cyst. PathologyOutlines.com [Available at: https://www.pathologyoutlines.com/topic/ovarynontumorfollicularcysts.html]

14.
Busca A, Parra-Herran C. Corpus luteum cyst. PathologyOutlines.com [Available at: https://www.pathologyoutlines.com/topic/ovarynontumorcorpuslutcyst.html]

15.
Abbas AM, Amin MT, Tolba SM, Ali MK. Hemorrhagic ovarian cysts: Clinical and sonographic correlation with the management options. Middle East Fertility Society Journal 2016;21(1):41–5. [CrossRef]

16.
Abduljabbar HS, Bukhari YA, Al Hachim EG, et al. Review of 244 cases of ovarian cysts. Saudi Med J 2015;36(7):834–8. [CrossRef]
[Pubmed]

17.
Jones KD. The prevalence and age distribution of ovarian cysts among women attending a London teaching hospital. J Obstet Gynaecol 2001;21(1):70–1. [CrossRef]
[Pubmed]

18.
Mobeen S, Apostol R. Ovarian Cyst. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
[Pubmed]

19.
20.
Hoyle AT, Puckett Y. Endometrioma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
[Pubmed]

21.
Teede H, Deeks A, Moran L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med 2010;8:41. [CrossRef]
[Pubmed]

22.
Venturoli S, Porcu E, Fabbri R, et al. Menstrual irregularities in adolescents: Hormonal pattern and ovarian morphology. Horm Res 1986;24(4):269–79. [CrossRef]
[Pubmed]

23.
24.
Madill M, Grabosch SM. Ovarian cyst [Internet]. Medscape; 2023. [Available at: https://emedicine.medscape.com/article/255865-overview?form=fpf]

25.
Grigore M, Murarasu M, Himiniuc LM, Toma BF, Duma O, Popovici R. Large ovarian tumors in adolescents, a systematic review of reported cases, diagnostic findings and surgical management. Taiwan J Obstet Gynecol 2021;60(4):602–8. [CrossRef]
[Pubmed]

26.
Khan N, Afroz N, Aqil B, Khan T, Ahmad I. Neoplastic and nonneoplastic ovarian masses: Diagnosis on cytology. J Cytol 2009;26(4):129–33. [CrossRef]
[Pubmed]

27.
Kanizsai B, Orley J, Szigetvári I, Doszpod J. Ovarian cysts in children and adolescents: Their occurrence, behavior, and management. J Pediatr Adolesc Gynecol 1998;11(2):85–8. [CrossRef]
[Pubmed]

28.
Winata IGS, Sabatini EP, Purnomo FS. Diagnosis and treatment of benign ovarian tumors. European Journal of Medical and Health Sciences 2022;4(2):1–3. [CrossRef]

29.
Kanani J, Sheikh MI. Undiagnosed, uncomplicated foreign body in abdominal cavity – A case of medical negligence. Surgery Case Reports 2024;2:100024. [CrossRef]

SUPPORTING INFORMATION
Acknowledgments
The authors wish to thank Mr. Alex Adeyemo, data analyst and statistician with the University of Abuja, Gwagwalada, Abuja, Nigeria, for his assistance with the data analysis. All relevant data are available upon reasonable request.
Author ContributionsBamnan Collins Dallang - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ijeoma Ahunna Okwudire-Ejeh - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Kevin Nwabueze Ezike - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Aminu M Mai - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Oluseyi A Asaolu - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shiktira D Kwari - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adewunmi Oluseye Adeoye - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Emmanuel Eyitayo Oguntebi - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Bamnan Collins Dallang et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.