|
Case Report
US and MRI contribution in non-puerperal uterine inversion: A case report
1 Department of Pediatric and OB & GYN Radiology, Faculty of Medicine, Hospital Ibn Sina, Rabat, Morocco
Address correspondence to:
Najwa Amsiguine
Department of Pediatric and OB & GYN Radiology, Faculty of Medicine, Hospital Ibn Sina, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100027G06NA2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Amsiguine N, Halfi MI, Najlae E, Allali N, Latifa C. US and MRI contribution in non-puerperal uterine inversion: A case report. Edorium J Gynecol Obstet 2022;7(2):1–4.ABSTRACT
Uterine inversion is a rare and potentially life-threatening complication. It is mainly of two types: puerperal and non-puerperal with further subdivision into complete and incomplete. Earlier diagnosis was crucial in order to avoid irreversible damage to the reproductive organs and adjacent structures. We present a case of a 45-year-old woman where the imaging diagnosis of her chronic pelvic pain fortuitously revealed a non-puerperal uterine inversion. This rare case emphasized the importance of a better understanding of the pelvic anatomy by radiologist in order to facilitate the comprehension of such pathologies with lost clear anatomy in imaging.
Keywords: MRI, Non-puerperal, Ultrasound, Uterine inversion
INTRODUCTION
Uterine inversion is an unpredictable serious complication of pregnancy. The reported incidence of puerperal complete uterine inversion ranges from 1 in 2000 to 1 in 30,000 deliveries. The etiology is a mismanaged third stage of labor [1]. Non-puerperal uterine inversions, as rare as they are, are reported to constitute 17% of all uterine inversions considered [2]. We present a case of a 45-year-old woman with antecedent of leiomyomectomy, presenting at the emergency room (ER) with pelvic pain and menorrhagia few years following the surgery.
CASE REPORT
A 45-year-old woman who had a full-term successful vaginal delivery and history of a huge fibroma that has been resected few years back, presented with pelvic pain and important vaginal bleeding that has been evolving chronical for the years following the surgery. The gynecology exam showed an unrecognizable cervical ring, the cervix opening was nowhere to be found and the rectal exam revealed an odd positioning of the uterus inside the pelvic cavity.
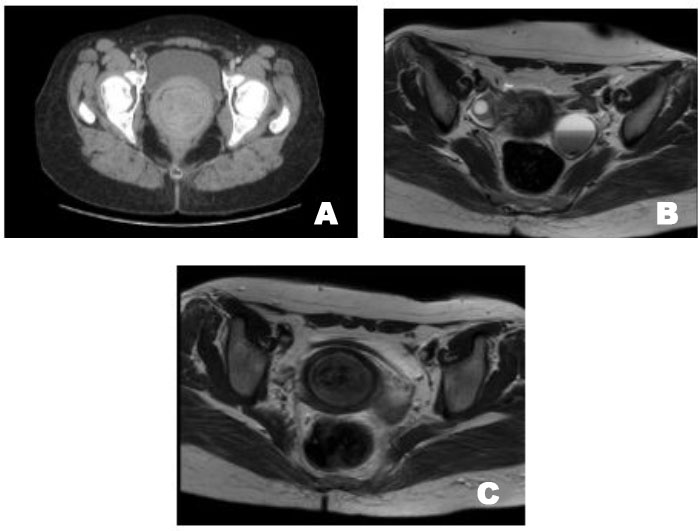
Initially ultrasound (US) and computed tomography (CT) scan did not show an intrauterine mass although the local anatomy of the uterus from its ligaments to its myoma was not well limited nor identified, which demanded to further complete the radiological investigation with magnetic resonance imaging (MRI).
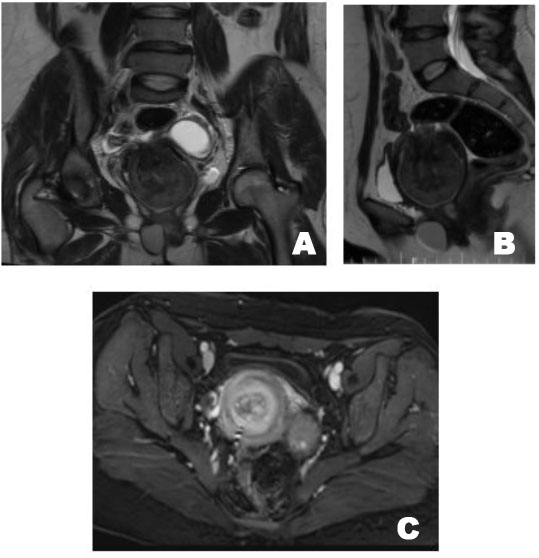
Magnetic resonance imaging helped putting the diagnosis of neglected complete uterine inversion in place showing a multi-layered concentric appearance of the uterus (“bull’s eye”) with a heterogeneous hyperintense mass occupying and enlarging the vaginal lumen (Figure 1 and Figure 2).
DISCUSSION
Non-puerperal uterine inversion (NPUI) is in 59% of cases associated to benign expansive tumors such as polyps or leiomyomas and to malignant tumors such as sarcomas in 32% of cases with a 9% idiopathic origin. In our case, the patient had undergone a surgical removal of a leiomyoma, the uterus was normally placed, therefore the idiopathic origin of this NPUI has been retained [2].
The etiology of the tumor-associated inversion includes many mechanisms, such as sudden extrusion of a rapidly growing tumor from the uterus, a thin uterine wall, dilatation of the uterine cervix, tumor size, fundic localization of the tumor, and a thin tumoral pedicle. Sarcoma-associated uterine inversion may be related to the softening of the uterine wall, due to tumor enlargement into the uterine cavity. Nulliparity, menopause, and intra-abdominal pressure secondary to cough or sneezing may also play a role in the reduction of the thickness of the uterine wall [3].
Although rare in advanced countries, it is important to remember such pathologies especially in low income countries where the access to healthcare is limited and therefore such pathologies emerge. Moreover, our case has no actual cause and no literature of similar case has been reported, in comprising with more mechanically cause inversion where the diagnosis is much easier.
The clinical symptoms are abdominal pain, vaginal hemorrhage urinary symptoms have also been described in some reports. Non-puerperal uterine inversion has been classified into three groups depending on the degree of the inversion [1],[2],[4].
Stage 1: Inversion of the uterus is intrauterine or incomplete. The fundus remains within the cavity.
Stage 2: A complete inversion of the uterine fundus through the fibromuscular ring of the cervix.
Stage 3: Total inversion, whereby the fundus protrudes through the vulva, here falls our case.
Stage 4: The vagina is also involved with complete inversion through the vulva along with the inverted uterus.
Although hard to identify for an unexperienced US user, three distinct findings are seen on sonography: mirror reflection, in which the inverted uterus is seen as a mirror image of the normally positioned uterus; pseudo-stripe, where two opposing serosal surfaces are seen as a hyperechoic stripe; target sign (bull’s eye sign), where the uterine fundus is seen in the center surrounded by a hyperechoic endometrium that is again surrounded by a hypoechoic rim representing fluid within the space between the uterine fundus and cervical/vaginal rim [1]. Further categorization of the inversion could be made depending on the shape of the uterine cavity on longitudinal plane: Y shape is seen in incomplete uterine inversion and U shape configuration reflects in a complete inversion [4].
Computed tomography scan has not been very useful in the diagnosis of NPUI, it may contribute in visualization of a low density material in the middle of the pelvis due to edematous endometrium and myometrium are features suggestive of uterine inversion. Some authors described the “target” sign while imaging the lower pelvis on axial images [4].
Magnetic resonance imaging is found to be sensitive in the diagnosis of NPUI. The distinct observations identified are U-shaped uterine cavity, a thickened and inverted uterine fundus on a sagittal section, and a “bull’s eye” configuration on the horizontal section (Figure 2B and Figure 2C). U-shaped cavity could also be noted even in cases of inversion due to pedunculated tumors. In complete inversion, identifying the round ligaments and fallopian tubes protruding centrally from the top of the uterus resembling the aspect of a vase with protruding flowers on top. Magnetic resonance imaging will further help in imaging lymph nodes [4] (Figure 1 and Figure 2).
The management of acute or chronic non-puerperal inversion uterus is surgical, which can be done via abdominal, vaginal, or laparoscopic routes. Many surgical procedures have been described to treat NPUI, each one is considered depending on the causative pathology, clinical presentation, desire for future fertility of the patient, and the surgical expertise. There are several different methods described in the literature: Huntington’s method, Haultain’s operation which seem to be the most successful, Spinell’s operation, and Kustner’s approach. In our case a conservative approach was settled on the will of the patient, therefore a hysterectomy was performed, revealing a uterus with few necrotic areas. Postoperatively, no complications were reported [5].
CONCLUSION
Non-puerperal uterine inversion is a rare clinical condition. Due to different presentations of the condition and the low incidence, it can be misdiagnosed on initial assessment. Leiomyomata are the common cause of uterine inversion, though a significant proportion was due to malignancies. Ultrasound and MRI have been used successfully in confirming the clinical diagnosis. Magnetic resonance study clearly documented uterine inversion in our case, which directly resulted in appropriate therapeutic intervention although the delayed consult of the patient that contributed further her complications.
REFERENCES
1.
Thakur S, Sharma S, Jhobta A, Aggarwal N, Thakur CS. Sonographic and MR features of puerperal uterine inversion. Jpn J Radiol 2014;32(6):356–9. [CrossRef]
[Pubmed]

2.
Duesberg M, Leconte I, Marbaix E, Squiffle J, Stainier A, Fellah L. Inversion utérine non puerpérale compliquée d”une nécrose vésicale. Journal D’imagerie Diagnosytique et Interventionnelle 2022;5(2):116–20. [CrossRef]

3.
Occhionero M, Restaino G, Ciuffreda M, Carbone A, Sallustio G, Ferrandina G. Uterine inversion in association with uterine sarcoma: A case report with MRI findings and review of the literature. Gynecol Obstet Invest 2012;73(3):260–4. [CrossRef]
[Pubmed]

4.
Herath RP, Patabendige M, Rashid M, Wijesinghe PS. Nonpuerperal uterine inversion: What the gynaecologists need to know? Obstet Gynecol Int 2020;2020:8625186. [CrossRef]
[Pubmed]

5.
De A, Nigam A, Jain A, Gupta N, Tripathi R. Laparoscopic management of nonpuerperal uterine inversion. J Minim Invasive Gynecol 2019;26(5):981–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Najwa Amsiguine - Conception of the work, Design of the work, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohamed Ismail Halfi - Conception of the work, Design of the work, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Elghorfi Najlae - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nazik Allali - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Chat Latifa - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Najwa Amsiguine et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.