|
Case Report
Intestinal incarceration following aspiration evacuation: A case report
1 Tunis el Manar University, Beja Maternity Center, Tunis, Tunisia
Address correspondence to:
Montacer Hafsi
Medical Resident in Gynecology and Obstetrics,
Tunisia
Message to Corresponding Author
Article ID: 100035G06MH2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Hafsi M, Moussi M, Zouaghi A, Rihani S, Najar S, Dridi F, Smaoui M, Mourali M. Intestinal incarceration following aspiration evacuation: A case report. Edorium J Gynecol Obstet 2024;9(1):5–8.ABSTRACT
Uterine perforation is a frequently overlooked complication of operative procedures. The incidence of perforation is estimated to range from 1 to 4 per 1000 during curettages for pregnancy termination. Reported complications include uterine, digestive, and vesical perforations, hemorrhage, endometritis, and secondary infertility. However, intestinal incarceration after uterine perforation remains extremely rare. We present a case of uterine perforation occurring after an aspiration curettage, complicated by digestive incarceration.
Keywords: Aspiration curettage, Digestive loop incarceration, Uterine perforation
INTRODUCTION
Operative management of failed medical treatment for terminated pregnancies often involves aspiration curettage. Complications of this procedure are infrequent but can range in severity from cervical tears to digestive injuries. The estimated complication rate is approximately 2%. Reported complications include uterine, digestive, and vesical perforations, hemorrhage, endometritis, and secondary infertility. The incidence of uterine perforation increases with gestational age, from 0.9 per 1000 in the first trimester to 3 per 1000 in the third trimester. Here, we report a case of uterine perforation post-aspiration curettage complicated by digestive incarceration. Based on this case, we discuss diagnostic criteria and the management of this complication.
CASE REPORT
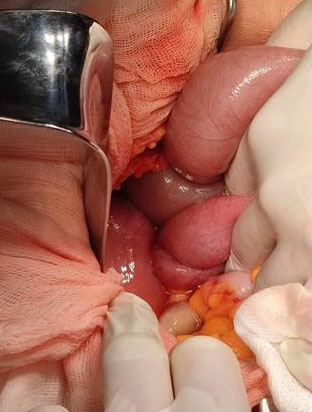
Patient D.A., a 29-year-old G4P3A0 (3AVB) with an unremarkable medical history, presented with post-Misoprostol bleeding following management of a terminated pregnancy, accompanied by severe anemia (2.8 g/dL). On examination, the patient exhibited fever (38.5°C), correct blood pressure (130/70 mmHg), and a heart rate of 140 bpm. Abdominal examination revealed a soft abdomen and vaginal examination displayed clotting bleeding originating from trophoblastic tissue. Ultrasound revealed a 3 cm heterogeneous retention image with no extrauterine mass or fluid (Figure 1). A diagnosis of hemorrhagic endometritis was established. The patient stabilization, antibiotic initiation, and transfusion of five units of cross-matched packed red blood cells were performed, resulting in a post-transfusion hemoglobin level of 7.8 g/dL. Aspiration of trophoblastic products under ultrasound guidance in the operating room resulted in minimal bleeding of intrauterine origin at the end of the procedure (Figure 2, Figure 3, Figure 4, Figure 5).
Postoperative evolution was marked by vomiting 14 hours postoperatively. The patient remained afebrile, hemodynamically stable, with a soft abdomen initially but progressed to abdominal pain, distension, cessation of bowel movements and gas, and recurrent vomiting after 5 hours. Abdominal X-ray revealed diffuse hydro-aerial levels and pelvic ultrasound demonstrated a moderate to abundant fluid collection.
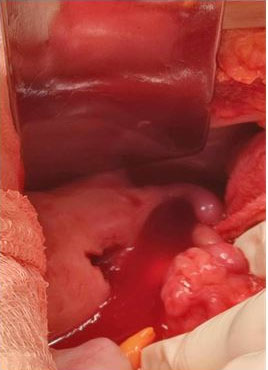
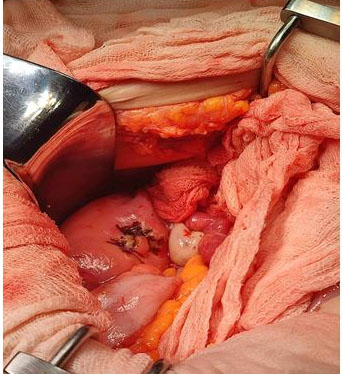
An abdominal computed tomography (CT) scan confirmed uterine perforation with a strangulated intestinal loop. The patient was urgently taken to the operating room, where intraoperative exploration revealed intestinal incarceration through a 2 cm fundal uterine perforation with viable intestines.
A 4 cm deperitonization was sutured with simple stitches at V1_zero, uterine perforation was sutured, and peritoneal lavage was performed.
Postoperative recovery was uneventful, with bowel movement restored on postoperative day 2, and discharge on day 7.
DISCUSSION
Uterine perforation is often underestimated, with an estimated incidence of 1 to 4 per 1000 during curettages for terminated pregnancies. Risk factors include surgeon inexperience, gestational age, and early postpartum period [1]. Perforations most commonly occur at the fundus, uterine horns, and anterior wall. While bladder and digestive injuries are potential complications, intestinal incarceration following uterine perforation is exceedingly rare [2].
Risk factors for digestive loop incarceration include perforation diameter, clandestine abortions, curettage for molar pregnancies, and multiple pregnancies. Clinical symptoms may be delayed, and common manifestations include vomiting, abdominal pain, distension, and cessation of bowel movements and gas [3]. Peritonitis is the most frequent complication after uterine perforation, presenting with a distended and tender abdomen.
Abdominal X-ray is the primary diagnostic tool, displaying hydro-aerial levels. Ultrasound may reveal a hyper-echogenic tubular structure within the uterus, with peristaltic movements, hypo- or hyper-echoic content, and sometimes hydro-aerial levels [4]. Computed tomography scans confirm the diagnosis.
Surgical intervention is the standard treatment for digestive loop incarceration. The management of uterine perforations post-aspiration curettage is not standardized, with either conservative or interventional approaches [5]. If the patient is stable and asymptomatic, observation with close monitoring may be an option. Some teams advocate for systematic exploratory laparoscopy [6]. Minimal perforations without bleeding may require no intervention, while extensive and hemorrhagic perforations can be managed by bipolar coagulation or suturing [7].
Uterine perforation can impact fertility through cervical stenosis or synechiae and increases the risk of ectopic pregnancies at the perforation site and uterine rupture [8]. Delivery mode should be carefully considered in subsequent pregnancies. In our case, the patient conceived one year postoperatively and delivered vaginally without rupture or cavity compromise [9].
CONCLUSION
Complications of uterine perforation can jeopardize the patient’s life. While rare, digestive incarceration is an exceptional but surgically urgent complication. Surgeon experience is crucial in preventing such complications. Ultrasound-guided procedures can provide added safety, particularly for less experienced practitioners.
REFERENCES
1.
Amarin ZO, Badria LF. A survey of uterine perforation following dilatation and curettage or evacuation of retained products of conception. Arch Gynecol Obstet 2005;271(3):203–6. [CrossRef]
[Pubmed]

2.
Koutélé F, Nicolas K, Rivière MF, Ledoux A. About two cases of uterine rupture outside of labour: Consequences of an unnoticed previous perforation. [Article in French]. Gynecol Obstet Fertil 2003;31(4):362–4. [CrossRef]
[Pubmed]

3.
Leibner EC. Delayed presentation of uterine perforation. Ann Emerg Med 1995;26(5):643–6. [CrossRef]
[Pubmed]

4.
Joint Study of the Royal College of General Practitioners and the Royal College of Obstetricians and Gynaecologists. Induced abortion operations and their early sequelae. J R Coll Gen Pract 1985;35(273):175–80.
[Pubmed]

5.
Dunner PS, Thomas MA, Ferreras M, Jerome M. Intrauterine incarcerated bowel following uterine perforation during an abortion: A case report. Am J Obstet Gynecol 1983;147(8):969–70. [CrossRef]
[Pubmed]

6.
Grimes DA, Schulz KF, Cates W Jr, Tyler CW Jr. Local versus general anesthesia: Which is safer for performing suction curettage abortions? Am J Obstet Gynecol 1979;135(8):1030–5. [CrossRef]
[Pubmed]

7.
Maglinte DD, Gage SN, Harmon BH, et al. Obstruction of the small intestine: Accuracy and role of CT in diagnosis. Radiology 1993;188(1):61–4. [CrossRef]
[Pubmed]

8.
Ka I, Diop PS, Niang AB, Faye A, Ndoye JM, Fall B. Acute generalized peritonitis due to uterine perforation following abortion: Case study observation. [Article in French]. Pan Afr Med J 2016;24:98. [CrossRef]
[Pubmed]

9.
Shulman SG, Bell CL, Hampf FE. Uterine perforation and small bowel incarceration: Sonographic and surgical findings. Emerg Radiol 2006;13(1):43–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Montacer Hafsi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marwa Moussi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Asma Zouaghi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sarra Rihani - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Souhir Najar - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Faten Dridi - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Maroua Smaoui - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mechaal Mourali - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Montacer Hafsi et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.