|
Case Report
Umbilical endometriosis: A case report
1 Department of Gynecology, IBN Rochd University Hospital, Casablanca, Morocco
Address correspondence to:
Rachida Sabiri
Service de Gynecologie, Aile 8, Chu IBN Rochd, Casablanca,
Morocco
Message to Corresponding Author
Article ID: 100033G06RS2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sabiri R, Gourja Y, Benrahal S, Houssin B, Sakher M, Samouh N. Umbilical endometriosis: A case report. Edorium J Gynecol Obstet 2023;8(2):5–9.ABSTRACT
Introduction: Cutaneous and umbilical involvement is very rare and represents only 0.5–1% in the various series. Its clinical diagnosis is difficult but it should be suspected in the presence of any bluish, painful umbilical nodule, sometimes with a brownish discharge, the evolution regulated by the menstrual cycle. Ultrasound of the abdominal wall points to the diagnosis of umbilical endometriosis despite the absence of characteristic signs on imaging. Wide surgical excision is the treatment of choice because of its resemblance to a primary tumor or metastasis.
Case Report: We report the case of a 31-year-old female patient with no history of abdominal-pelvic surgery or trauma to the umbilicus, consulted for a painful umbilical swelling measuring approximately 1–2 cm diagnosed with umbilical endometriosis. Endometriosis of the umbilical wall is a rare condition, representing only 0.03–2% of extra-genital endometriosis. It is associated with pelvic endometriosis in 26% of cases. Its clinical diagnosis is difficult but it should be suspected in the presence of any bluish, painful umbilical nodule, sometimes with a brownish discharge, the evolution regulated by the menstrual cycle. Ultrasound of the abdominal wall with a high frequency probe is the initial, easily accessible examination that points to the diagnosis of umbilical endometriosis, but it is not pathognomonic. The formal diagnosis of umbilical endometriosis is only obtained with the help of histological examination. The presence of endometrial glands (epithelial cells) and a cytogenic chorion in the ectopic endometrial tissue is necessary to establish the histological diagnosis. In general, medical treatment with danazol, norethisterone, or luteinizing hormone-releasing hormone (LHRH) analogues is recommended before surgery. It would allow a reduction in the size of the endometriotic nodules.
Conclusion: Umbilical endometriosis is a very rare form of extra-genital endometriosis. The diagnosis is made when a nodule is present with pain and catamenial bleeding. The diagnosis of certainty is based on a histological study.
Keywords: Cutaneous, Endometriosis, Nodule, Umbilical
INTRODUCTION
Endometriosis is a condition characterized by the presence of ectopic endometrial structures which have the histological and biological characteristics of the endometrium, but which remain anatomically separate from it. It affects women during their genital period [1]. Cutaneous and umbilical involvement is very rare and represents only 0.5–1% in various series.
Two types of umbilical endometriosis can be distinguished, the pathophysiology of which still remains a challenge for research. The primary form appears on an abdomen unaffected by any surgical intervention and the secondary form on a scar following a gyneco-obstetric intervention or laparoscopy [2]. Its clinical diagnosis is difficult but it should be suspected in the presence of any bluish, painful umbilical nodule, sometimes with a brownish discharge, the evolution regulated by the menstrual cycle. Ultrasound of the abdominal wall points to the diagnosis of umbilical endometriosis despite the absence of characteristic signs on imaging. Wide surgical excision is the treatment of choice because of its resemblance to a primary tumor or metastasis. We report a case of umbilical endometriosis explored by ultrasound. Through the analysis of this rare observation, we highlight the difficulties related to clinical and ultrasound diagnosis and advanced theories of the pathophysiology of umbilical endometriosis [3].
CASE REPORT
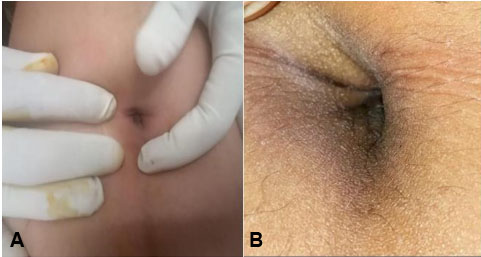
A 31-year-old woman, multiparous, with no history of abdominal-pelvic surgery or trauma to the umbilicus, consulted for a painful umbilical swelling measuring approximately 1–2 cm, which had been evolving for two years, becoming purplish and sensitive at the beginning of menstruation (Figure 1B), causing a minimal discharge of brownish fluid, and appears thick at the end. She had been experiencing mild dysmenorrhea for several years, with inconstant deep dyspareunia.
On clinical examination, a bluish nodule about 1 cm in diameter was found at the bottom of the umbilical depression, which was tender to palpation (Figure 1A). The rest of the abdominal examination was normal.
The gynecological examination was normal. The cyclical nature of the bleeding and the symptomatology, which was accompanied by menstruation, made us suspect a primary umbilical endometriosis.
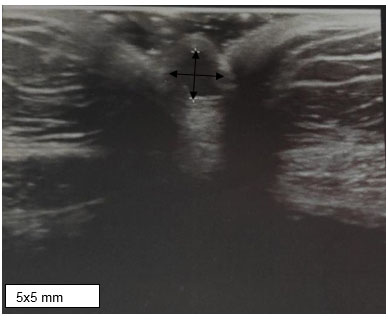
Ultrasound of the abdominal wall: skin thickening at the level of the umbilicus with a 5 mm umbilical nodule, well limited and finely echogenic, suggesting an endometrial nodule (Figure 2).
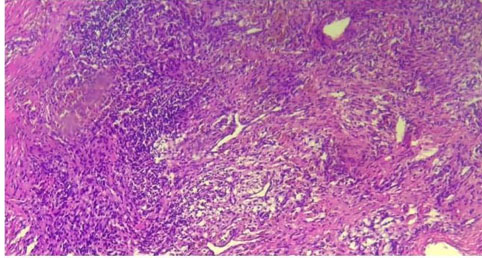
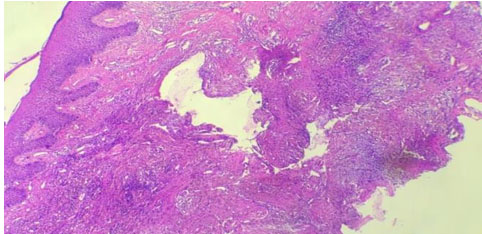
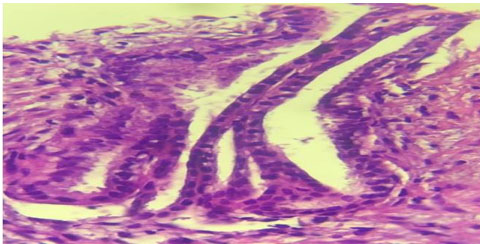
Pelvic magnetic resonance imaging (MRI) examination did not identify any lesions of pelvic endometriosis. Skin histology showed papillomatous acanthotic epidermis with orthokeratosis. The dermis has an interstitial infiltrate with siderophages and hemosiderin deposits. With the presence of a glandular structure partially represented as a regular cubocylindrical epithelium without atypia (Figure 3, Figure 4, Figure 5). The diagnosis of primary umbilical endometriosis is retained.
As a result, treatment with leuprolide acetate was instituted and surgical removal was recommended as a secondary procedure. After one month of leuprolide (LHRH analogue), the patient noted a disappearance of menstrual symptoms (pain, bleeding, and abdominal swelling) and she is awaiting surgery after two months of treatment.
DISCUSSION
Endometriosis is characterized by the presence of functional endometrial tissue outside the uterine cavity, and skin involvement is very rare, representing only 0.5–1% in various series. It affects 15% of women in the genitally active period between the ages of 20 and 40 and 5% of cases are discovered in postmenopausal women. The usual locations of endometriosis are ovarian, peritoneal, in the partition separating the bladder, the uterus, and the vagina or the rectum [3].
A distinction is made between internal endometriosis or adenomyosis, which is the implantation of endometrial cells in the myometrium, and external endometriosis, which is the location of endometriotic tissue outside the myometrium and endometriotic tissue outside the uterine cavity and myometrium.
Extra-genital locations are thought to represent 5% of lesions and seem to be underestimated in the literature. The existence of these lesions often calls for different physiopathological theories to explain their extra-pelvic location [1]. The lesions may be multiple or single, with a wide variety of sites. Diagnosis can be difficult due to the atypical and unexpected symptoms described by patients. However, the catamenial nature of the pain or symptoms is a characteristic and highly suggestive feature regardless of location. It is essential to make the diagnosis, as these conditions can also have a real impact on the patient’s health and quality of life [4].
Endometriosis of the abdominal wall, particularly the umbilicus is a rare condition, representing only 0.03–2% of extra-genital endometriosis. It is associated with pelvic endometriosis in 26% of cases.
Two types of umbilical endometriosis can be distinguished: primary endometriosis, which is exceptional, occurs in women with no history of abdominal surgery, and secondary endometriosis, which is uncommon, appears on a scar following a gyneco-obstetric operation or on the site where the laparoscopic trocar passes [5].
The umbilical location could also be explained by the venous or lymphatic metastatic theory, when endometriotic cells migrate to the umbilicus through the periumbilical venous network. Finally, according to a third theory, that of metaplasia, cells derived from the coelomic epithelium undergo metaplasia toward endometrial cells, under the effect of various infectious, toxic, or hormonal factors [6].
The most common differential diagnoses with umbilical endometriosis include umbilical hernia, primary malignancy such as melanoma or metastasis, lipoma, inflammatory or infectious granuloma, complicating cyst, congenital cyst of the urachus and endometriosis [7]. Umbilical hernia is a real dilemma in acute abdominal symptomatology, as in the case of our patient. Ultrasound of abdominal wall with a high frequency probe is the initial, easily accessible examination that points to the diagnosis of umbilical endometriosis, but it is not pathognomonic. It confirms the presence of an umbilical nodule, specifies its size, its contours, its limits with the adjacent superficial and deep structures, its homo or heterogeneous content, its solid or cystic nature [8].
Endometriosis of the abdominal wall, particularly the umbilical wall, is a rare condition, representing only 0.03–2% of extra-genital endometriosis. It is associated with pelvic endometriosis in 26% of cases.
Percutaneous biopsy of the nodule evokes the diagnosis by showing a cylindrical glandular epithelium surrounded by a stroma. A study by Catalina-Fernandez et al. showed that in cytological smears of cutaneous endometriosis there is a high cellularity containing macrophages loaded with hemosiderin and epithelial cells on old bleeding. It is still contraindicated by some authors because of the increased risk of dissemination in cases of suspected endometriosis [7].
Finally, the formal diagnosis of umbilical endometriosis is only obtained with the help of histological examination. The presence of endometrial glands (epithelial cells) and a cytogenic chorion in the ectopic endometrial tissue is necessary to establish the histological diagnosis. It consists of small foci of inflamed endometrial tissue and hemosiderin-laden macrophages secondary to acute and chronic bleeding. The typical histological appearance of endometriosis excludes a primary malignant tumor, umbilical metastasis, or a benign lesion [4].
The treatment for umbilical endometriosis is wide surgical excision because of its similarity to malignant tumors and to avoid recurrence. Malignant transformation into carcinoma of endometriotic nodules is rare.
In general, medical treatment with danazol, norethisterone, or LHRH analogues is recommended before surgery. It would allow a reduction in the size of the endometriotic nodules [9].
CONCLUSION
Umbilical endometriosis is a rare, atypical form of extra-genital endometriosis. The diagnosis should be made in the presence of cyclical symptomatology, enabling a therapeutic protocol to be instituted after histological confirmation.
REFERENCES
1.
Tropicale TS. Santé Maghreb - Bibliothèque de Santé Maghreb. APIDPM Santé Tropicale. 2021. [Available at: http://www.santemaghreb.com/biblio.asp?id=1951&action=lire]

2.
Darouichi M. Endométriose ombilicale primitive et secondaire. Feuillets de Radiologie 2013;53(1):59. [CrossRef]

3.
Mohamed A, Brahmi YE, Mouhafid FE, et al. Endométriose de la paroi abdominale antérieure: à propos d´un cas et revue de la littérature. PAMJ - Clinical Medicine 2020;4(65). [CrossRef]

4.
5.
Rubegni P, Sbano P, Santopietro R, Fimiani M. Case 4. Umbilical endometriosis. Clin Exp Dermatol 2003;28(5):571–2. [CrossRef]
[Pubmed]

6.
Abramowicz S, Pura I, Vassilieff M, et al. Endométriose ombilicale chez les femmes sans antécédents chirurgicaux. Journal de Gynécologie Obstétrique et Biologie de la Reproduction 2011;40(6):572–6. [CrossRef]

7.
Catalina-Fernández I, López-Presa D, Sáenz-Santamaria J. Fine needle aspiration cytology in cutaneous and subcutaneous endometriosis. Acta Cytol 2007;51(3):380–4. [CrossRef]
[Pubmed]

8.
Merlot B, Ploteau S, Abergel A, et al. Extragenital endometriosis: Parietal, thoracic, diaphragmatic and nervous lesions. CNGOF-HAS Endometriosis Guidelines. [Article in French]. Gynecol Obstet Fertil Senol 2018;46(3):319–25. [CrossRef]
[Pubmed]

9.
Malic CC, Spyrou GE, Hough M, Fourie L. Patient satisfaction with two different methods of umbilicoplasty. Plast Reconstr Surg 2007;119(1):357–61. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Rachida Sabiri - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yasmine Gourja - Conception of the work, Design of the work, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sanaa Benrahal - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Boufettal Houssin - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mahdaoui Sakher - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Naima Samouh - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Rachida Sabiri et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.