|
Case Report
Alobar holoprosencephaly: A case report
1 Professor in Obstetrics and Gynecology Department, University Hospital Center Ibn Rochd, Casablanca 20100, Morocco
2 Resident Doctor in Obstetrics and Gynecology Department, University Hospital Center Ibn Rochd, Casablanca 20100, Morocco
3 Head of Service in Obstetrics and Gynecology Department, University Hospital Center Ibn Rochd, Casablanca 20100, Morocco
Address correspondence to:
Imane El Abbassi
Department of Gynecology and Obstetrics, University Hospital Center Ibn Rochd, Casablanca, Morocco; Faculty of Medicine and Pharmacy, Hassan II University, 1 rue des hôpitaux, Casablanca,
Morocco
Message to Corresponding Author
Article ID: 100032G06MJ2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Jalal M, El Abbassi I, Amghar A, Lamrissi A, Bouhya S. Alobar holoprosencephaly: A case report. Edorium J Gynecol Obstet 2023;8(2):1–4.ABSTRACT
Introduction: Holoprosencephaly (HPE) is a rare brain malformation, which results from a cleavage defect of the prosencephalon. Three forms have been described as: alobar, semi-lobar, and lobar forms.
Case Report: We report a rare case of holoprosencephaly, diagnosed at the maternity of the Ibn Rochd Hospital Center in Casablanca.
Conclusion: Holoprosencephaly is secondary to a cleavage anomaly of the prosencephalon, the diagnosis is based on echotomography, computed tomography (CT) scan and nuclear magnetic resonance imaging (MRI). It is important to perform a karyotype to look for a chromosomal anomaly. Holoprosencephaly, although rare, should be recognized and diagnosed; minor forms are likely to benefit from medical replacement therapy or ventricular shunting.
Keywords: Case report, Cerebral and facial malformations, Holoprosencephaly, Ultrasound transfontanellar
INTRODUCTION
Holoprosencephaly (HPE), formerly called arhinencephaly, covers a group of cerebral and facial malformations resulting from a diverticulation disorder. It includes three classical forms, of which the alobar form is the most severe, and results from a lack of longitudinal cleavage of the cerebral hemispheres [1],[2], with a poor prognosis. The objective is to report, through this observation, its clinical and evolutionary aspects.
CASE REPORT
Daughter of Mrs. F.L., newborn at term, female, last of three siblings, from a non-consanguineous marriage of a known diabetic mother under insulin, 38 years old, and from a poorly followed pregnancy estimated at term not supplemented in folic acid, and having taken fenugreek during the first trimester of her pregnancy was admitted in intensive care unit (ICU) at 6 hours of life, in a picture of fetal suffering, following a delivery by cesarean section. During her gestation, serology was performed at 28 weeks of amenorrhea: toxoplasmosis, rubella, and syphilis, but came back negative, as well as a single obstetrical ultrasound done at 28 weeks of amenorrhea (Figure 1), which suspected an anomaly of the ventricular system and then the patient was lost from sight until the day of her delivery.
On admission to the intensive care unit (ICU), the examination revealed axial hypotonia, with a cranial perimeter of 46 cm (+4 DS), cyclopia, syndactyly, and exencephaly. Archaic reflexes were present and the rest of the examination was unremarkable (Figure 2).
DISCUSSION
Holoprosencephaly is rare, occurring during the second month of embryonic life and is the most frequent malformation of the brain and face. It is secondary to a cleavage anomaly of the prosencephalon and is characterized by the formation of a median hemispheric mass [1]. Fenugreek is among the oldest medicinal and culinary plants. It is widely used as an herbal medicine in Morocco and the Mediterranean area. The Moroccan Pharmacovigilance Centre reported the early adverse events related to the consumption of this plant between March and August 2006. A lot of studies have subsequently confirmed the relationship between the consumption of fenugreek during pregnancy and the appearance of neural tube defects [2].
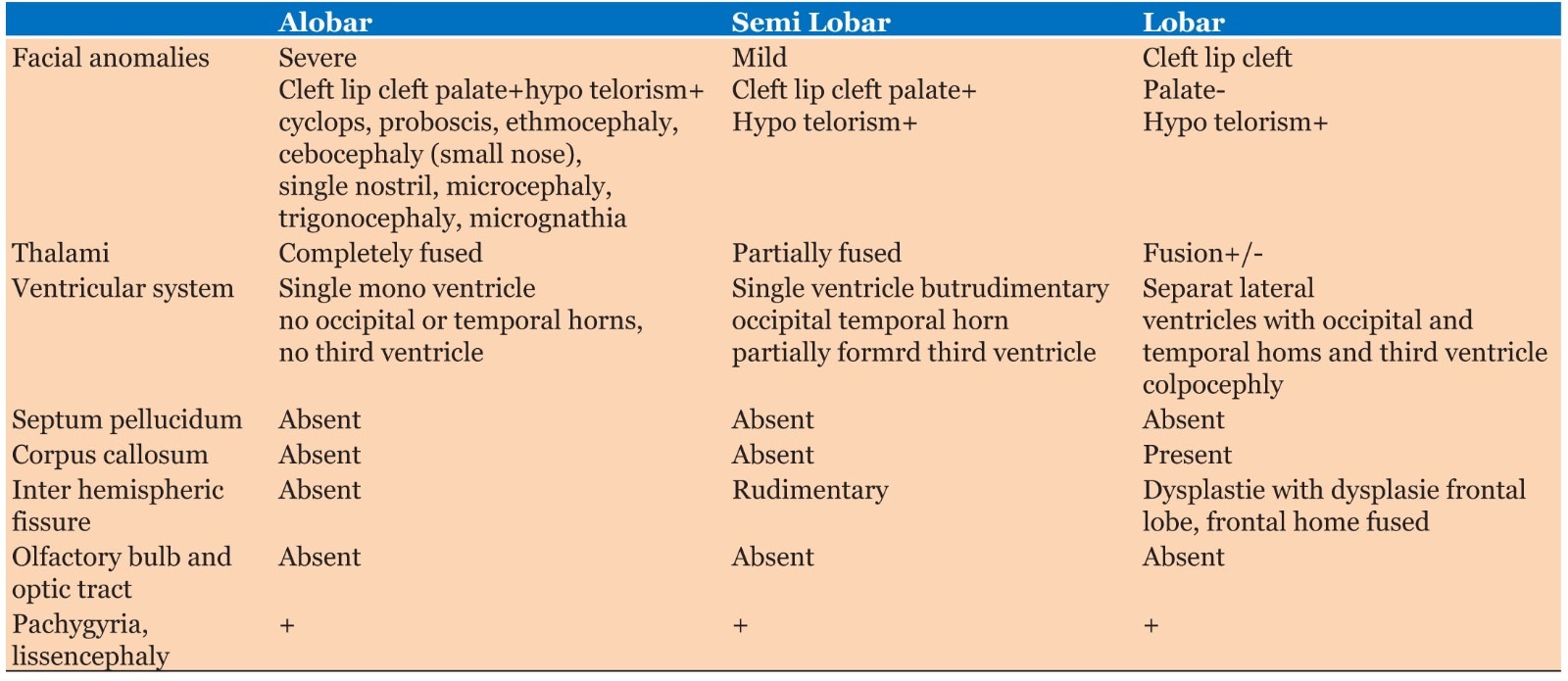
Several classifications have been proposed, but among them De Myer and Zeman are the most commonly used. It distinguishes three types of increasing severity: alobar, semi-lobar, and lobar holoprosencephaly [1],[3] (Table 1).
This condition can be grouped into three syndromes [1],[4]:
- A dysmorphic inconstant syndrome, frequently encountered in alobar holoprosencephaly of the type of cyclopia, ethmocephaly, cebocephaly, median or bilateral cleft lip or hypertelorism but which may be missing in 20% of cases. The severity of facial lesions reflects that of cerebral malformations for De Meyer and Zeman [4],[5] .
- A neurological syndrome: apnea and tonic spasms with axial hypotonia and spasticity of the limbs on An endocrine syndrome such as ante- or post-pituitary insufficiency [4],[5].
The prevalence of this condition is variously estimated to be between 1/5000 and 1/16,000 births, depending on whether or not one counts the frustrated forms that go unnoticed and the very severe forms that are incompatible with life. Among the risk factors, consanguinity, smoking and insulin-dependent diabetes in the mother would multiply the risk by 200 [1],[2].
These environmental parameters are risk factors for holoprosencephaly (HPE), but chromosomal abnormalities are found, with trisomy 13 and trisomy 18 in the forefront. There are alterations in 11 chromosomes likely to contain the genes responsible for HPE with diverse and complex malformations. This is a reminder of the importance of antenatal screening [3].
The diagnosis of holoprosencephaly is based primarily on imaging. Antepartum and transfontanellar ultrasonography performed in infants can guide the diagnosis, which will be confirmed by computed tomography (CT) scan or magnetic resonance imaging (MRI). An angiographic study may also be helpful [1],[5].
The brain is small and contains a single ventricular cavity (representing the third ventricle and lateral ventricles). A fluid pocket called “dorsal sac,” of variable size, communicating widely with the ventricular cavity. Facial malformations are often more complex. The characteristics of the CT scan of the brain are: it is a large single ventricular cavity, it is limited at the back by a membrane, and it is bordered at the front by a horseshoe-shaped brain parenchyma. The third ventricle is not individuated, and the basal ganglia are fused on the median line. At the sub-tensor level, the brainstem, the fourth ventricle and the cerebellum are present, either normal or hypoplastic and malformed (cyst). Angiography shows anomalies of the gyration, especially, a single anterior cerebral artery [1],[6].
The realization of the fetal karyotype is essential. The karyotype may be normal or present aneuploidies of number or structure. Among the genetic abnormalities, the most frequently associated with HPE include trisomies 13, 18, and 21 [7].
The study of the karyotype of the parents is also necessary, because if one of them presents a balanced anomaly the risk of recurrence is high, hence the need for a study of the fetal karyotype in case of a new gestation [6],[8].
CONCLUSION
Holoprosencephaly, although rare, should be recognized and diagnosed; minor forms are likely to benefit from medical replacement therapy or ventricular shunting. Antenatal screening is indicated in the case of a large pregnancy after a case of holoprosencephaly: fetal ultrasound and possibly karyotype. Thus, parents should be careful if another pregnancy is envisaged.
REFERENCES
1.
2.
Es Seddiki A, Messaouidi S, Amrani R. Le rôle du fenugrec dans la survenue d’anomalie de fermeture du tube neural: Un signal d’alerte depuis le Maroc. Phytothérapie 2017;15:155–8. [CrossRef]

3.
Seck N, Basse I, Keita Y, et al. Alobar holoprosencephaly associated with diabetes insipidus and hypothyroidism in a 10-month old infant. [Article in French]. Pan Afr Med J 2017;28:193. [CrossRef]
[Pubmed]

4.
Amadou DA, Franck D, Mamadou M, Mourtalla KM. Holoprosencephaly alobar amid polymalformative syndrome: Contribution of imaging in a case report. [Article in French]. Pan Afr Med J 2013;15:83. [CrossRef]
[Pubmed]

5.
Orioli IM, Castilla EE. Epidemiology of holoprosencephaly: Prevalence and risk factors. Am J Med Genet C Semin Med Genet 2010;154C(1):13–21. [CrossRef]
[Pubmed]

6.
Kruszka P, Muenke M. Syndromes associated with holoprosencephaly. Am J Med Genet C Semin Med Genet 2018;178(2):229–37. [CrossRef]
[Pubmed]

7.
8.
Raam MS, Solomon BD, Muenke M. Holoprosencephaly: A guide to diagnosis and clinical management. Indian Pediatr 2011;48(6):457–66. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Mohammed Jalal - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Imane El Abbassi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ayoub Amghar - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Amine Lamrissi - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Said Bouhya - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Mohammed Jalal et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.