|
Case Report
Sister Mary Joseph’s nodule revealing an ovarian adenocarcinoma: A case report
1 Gynecologic Department, Centre Hospitalier Universitaire Ibn Rochd, Faculté de Médecine et Pharmacie, Université Hassan II de Casablanca, Casablanca, Morocco
Address correspondence to:
Hlaibi Omnia
Centre Hospitalier Universitaire Ibn Rochd, Faculté de Médecine et Pharmacie, Université Hassan II de Casablanca, Casablanca,
Morocco
Message to Corresponding Author
Article ID: 100031G06FI2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Issam F, Zineb S, Omnia H, Houssin B, Sakher M, Naima S. Sister Mary Joseph’s nodule revealing an ovarian adenocarcinoma: A case report. Edorium J Gynecol Obstet 2023;8(1):8–11.ABSTRACT
Introduction: Sister Mary Joseph nodule is an eponymous term for a malignant metastatic umbilical nodule. It is a rare but important physical finding because it is indicative of advanced malignancy. The primary tumor is usually an adenocarcinoma, rarely a squamous cell carcinoma, melanoma, or sarcoma.
Case Report: We report the clinical case of a 64-year-old woman with metastatic ovarian adenocarcinoma and umbilical cutaneous metastasis. The diagnosis was established upon the umbilical node biopsy in April 2020, after the patient presented with an abdominal distension and respiratory difficulties.
Conclusion: Umbilical skin metastases are rare, and they are associated with advanced metastatic disease and a very poor prognosis. Through this work we try to clarify the mechanisms and the prognosis of this rare manifestation, and put the point on the importance of an early diagnosis.
Keywords: Ovarian adenocarcinoma, Sister Mary Joseph nodule, Umbilical metastasis
INTRODUCTION
Sister Mary Joseph nodule is an eponymous term for a malignant metastatic umbilical nodule. It is a rare but important physical finding because it is indicative of advanced malignancy [1]. It was described by Sister Marie Joseph Dempsey, an operating nurse at William J. Mayo in Rochester, Minnesota. The primary tumor is usually an adenocarcinoma, rarely a squamous cell carcinoma, melanoma, or sarcoma. It often occurs in a patient with a known cancer or reveals it. It is a very rare pathology and poses a double diagnostic and prognostic problem because cutaneous umbilical metastases of visceral tumors are not frequent [2].
We report a case of an umbilical skin metastasis revealing an ovarian adenocarcinoma in a patient admitted for abdominal distension causing respiratory discomfort at the Gynecology Department (department number 8) of the CHU Ibn Rochd of Casablanca, Morocco.
CASE REPORT
An 84-year-old patient, mother of two children born by vaginal delivery, diabetic on insulin for 20 years, hypertensive on renin angiotensin antagonist, who consulted for abdominal distension of progressive installation evolving since 08 months causing respiratory discomfort. The clinical examination objectified a patient with alteration of the general state, a distended abdomen with collateral venous circulation and declive dullness. There was also a painless subcutaneous umbilical nodule of 1 cm (Figure 1). The histological and immunohistochemical study of the biopsy was in favor of a metastasis of an adenocarcinoma of ovarian origin.
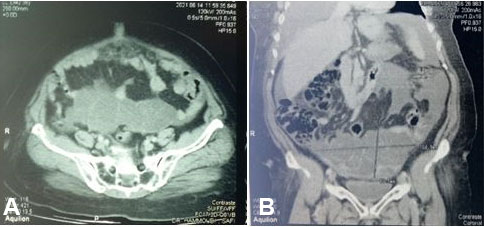
Moreover, the radiological work-up revealed an umbilical nodule associated with a solidocystic abdominal-pelvic mass with multiple partitions of probable ovarian origin with peritoneal carcinosis (Figure 2). The tumor markers requested: CA125 were elevated to 256 IU/L. The patient was presented at a multidisciplinary consultation meeting (RCP) with a decision to undergo palliative chemotherapy.
DISCUSSION
The Sister Mary Joseph nodule is a palpable nodule of the umbilicus most often secondary to a metastasis of an abdomino-pelvic cancer [2]. Its incidence is low, since it is estimated that 1–3% of patients with abdomino-pelvic neoplasia may have a Sister Mary Joseph nodule [3]. The discovery of this nodule poses the diagnostic and prognostic problem because the search for the primary tumor is not always easy [4].
The most common histological types of umbilical metastases are adenocarcinomas (90%) [5], but it may also (rarely) be squamous cell carcinoma or undifferentiated cancer [6]. The pathophysiology of the Sister Mary Joseph nodule is still incompletely elucidated. Indeed, there are four possible routes of dissemination of neoplastic cells to the umbilicus which are: hematogenous dissemination, extension from the hepatic round ligament to the middle umbilical ligament, retrograde lymphatic reflux, and contiguous dissemination from the anterior surface of the peritoneum via the dermal vessels of the umbilicus, which explains the appearance of the Sister Mary Joseph nodule in the advanced stages of deep cancers often accompanied by peritoneal carcinosis [5]. This nodule presents as a rounded, irregular, indurated swelling, often painful and oozing, sometimes pruritic. It may be of different colors: white, purple, red, brown. It usually measures between 5 and 20 mm in diameter, but can reach up to 10 cm [7]. The discovery of such a nodule must imperatively lead to an abdominal-pelvic computed tomography (CT) scan and a biopsy of the lesion in order to obtain an anatomopathological diagnosis [8]. The differential diagnosis is with benign tumors (endometriosis, melanocytic nevus, dermatofibroma, uracic cyst, seborrheic keratosis, pyogenic granuloma, omphalitis, keloid, foreign body, abscess, or even hernia) and malignant (melanoma, basal cell carcinoma, squamous cell carcinoma, myosarcoma, primary adenocarcinoma) [9]. The presence of Sister Mary Joseph nodules usually means advanced metastatic cancer with a poor prognosis. This can be explained by the late discovery of the tumor pathology in resource-limited countries on the one hand, and on the other hand the discrete character of the nodule which can be trivialized [5]. The discovery of a metastatic nodule at the umbilical site almost certainly establishes the non-operable nature of the patient. From the point of view of prognosis, all authors agree that the presence of the Sister Mary Joseph nodule remains a pejorative element. The average survival at the time of diagnosis is estimated at 11 months [5]. The evolution of our patient was marked by the occurrence of a death after four months of diagnosis of the pathology.
CONCLUSION
An umbilical lesion must be taken seriously by the practitioner, as it represents a neoplasm in two-thirds of cases, being either a primary cancer or a metastatic disease. The Sister Mary Joseph nodule is a rare umbilical metastatic lesion. Its discovery should lead to an abdomino-pelvic CT scan and skin biopsy. This nodule is characterized by its late onset and has been associated with a poor prognosis.
REFERENCES
1.
Tso S, Brockley J, Recica H, Ilchyshyn A. Sister Mary Joseph’s nodule: An unusual but important physical finding characteristic of widespread internal malignancy. Br J Gen Pract 2013;63(615):551–2. [CrossRef]
[Pubmed]

2.
Gabriele R, Conte M, Egidi F, Borghese M. Umbilical metastases: Current viewpoint. World J Surg Oncol 2005;3(1):13. [CrossRef]
[Pubmed]

3.
Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D. Umbilical metastasis or Sister Mary Joseph’s nodule. Int J Dermatol 1998;37(1):7–13. [CrossRef]
[Pubmed]

4.
Touré PS, Tall CT, Dioussé P, et al. Sister Mary Joseph nodule revealing digestive and ovarian carcinoma: Report of 4 cases. [Article in French]. Pan Afr Med J 2015;22:269. [CrossRef]
[Pubmed]

5.
Palaniappan M, Jose WM, Mehta A, Kumar K, Pavithran K. Umbilical metastasis: A case series of four Sister Joseph nodules from four different visceral malignancies. Curr Oncol 2010;17(6):78–81. [CrossRef]
[Pubmed]

6.
Leyrat B, Bernadach M, Ginzac A, Lusho S, Durando X. Sister Mary Joseph nodules: A case report about a rare location of skin metastasis. Case Rep Oncol 2021;14(1):664–70. [CrossRef]
[Pubmed]

7.
Touraud JP, Lentz N, Dutronc Y, Mercier E, Sagot P, Lambert D. Umbilical cutaneous metastasis (or Sister Mary Joseph’s nodule) disclosing an ovarian adenocarcinoma. [Article in French]. Gynecol Obstet Fertil 2000;28(10):719–21. [CrossRef]
[Pubmed]

8.
Kluger N. Umbilical and periumbilical dermatoses. [Article in French]. Ann Dermatol Venereol 2014;141(3):224–35. [CrossRef]
[Pubmed]

9.
Chalya PL, Mabula JB, Rambau PF, McHembe MD. Sister Mary Joseph’s nodule at a university teaching hospital in northwestern Tanzania: A retrospective review of 34 cases. World J Surg Oncol 2013;11:151. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Faizi Issam - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sami Zineb - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hlaibi Omnia - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Boufettal Houssin - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mahdaoui Sakher - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Samouh Naima - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Faizi Issam et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.