|
Case Report
Incidental pregnancy luteoma: A case report
1 MD, PGY-3 resident, Pathology Department, Louisiana State University, Shreveport, LA, USA
2 PGY-3 resident, Pathology Department, Louisiana State University, Shreveport, LA, USA
3 Professor, Louisiana State University, Shreveport, LA, USA
4 Associate Professor, Louisiana State University, Shreveport, LA, USA
Address correspondence to:
James D Cotelingam
MD, 1501, Kings Hwy, Pathology Department, Shreveport, LA 71103,
USA
Message to Corresponding Author
Article ID: 100029G06JL2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Lee J, Afude JI, Cotelingam JD, Ong M. Incidental pregnancy luteoma: A case report. Edorium J Gynecol Obstet 2023;8(1):1–3.ABSTRACT
Introduction: Pregnancy luteoma is a physiologic pseudotumor of ovary because of hormonal influence during pregnancy. It will regress spontaneously after delivery. Awareness of this process will assist to get the correct diagnosis at the right clinical context and lead to the appropriate management and follow-up for the patient.
Case Report: This is a brief case report on a multiparous pregnant woman who underwent emergent cesarean section and found an incidental right ovarian mass. Cystectomy was done for pathological evaluation, and the histomorphology and immunohistochemistry suggested pregnancy luteoma. Neither the patient nor her infant did not manifest any sign and symptoms including virilization effect during the hospital stay.
Conclusion: The clinician and pathologist need to be aware of this physiological process in pregnant women and its possible complications.
Keywords: Incidental, Luteoma, Pregnancy
INTRODUCTION
Pregnancy luteoma is a variant of physiologic condition caused by the hormonal influence during pregnancy especially during third trimester in multiparous women. It will regress spontaneously after delivery. With the relevant clinical history and frozen section diagnosis can render the diagnosis of pregnancy luteoma. The follow up visits of both mother and baby were uneventful. Although it is benign, there are possible maternal and fetal complications which include torsion of ovarian mass and fetal adrenocortical hormone disturbance. Therefore, clinical and radiologic follow-up is warrant.
CASE REPORT
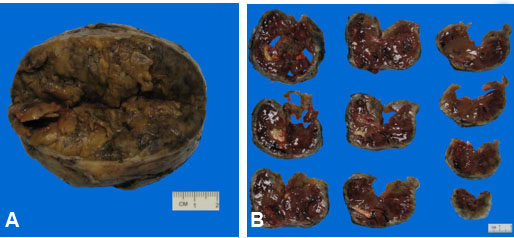
A 32-year-old gravida 4 para 3 female at 33-week gestation with history of pre-eclampsia, gestational diabetes mellitus and obesity presented to our institute with worsening pre-eclampsia. She underwent emergency cesarean section with delivery of a normal appearing preterm female infant. Intraoperatively, an incidental right ovarian mass was discovered, and cystectomy was performed. The postoperative period was uneventful. Gross examination of the ovarian cyst revealed a measurement of 8.2 × 6.6 × 5.1 cm, weight 186 grams, and a golden-brown external surface. The cut sections showed mostly solid—partially cystic components with a soft, yellow to tan, brown variegated appearance admixed with hemorrhage (Figure 1A and Figure 1B).
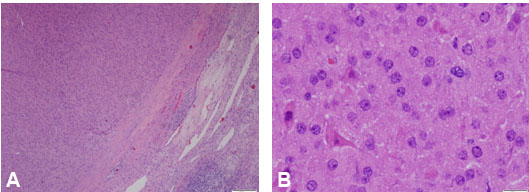
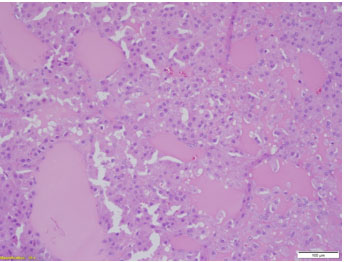
Microscopic examination revealed a well-encapsulated mass composed of sheets of monotonous cells with scant intervening stroma. The cells were large, oval to polygonal with eosinophilic granular cytoplasm, and bland looking nuclei. Some cells displayed prominent nucleoli (Figure 2A and Figure 2B). Follicular spaces filled with colloid-like secretions and focal areas of necrosis are observed (Figure 3).
The lesional cells are immunoreactive for androgen receptors, vimentin, calretinin, inhibin, Mart-1, Progesterone Receptor, and CD99. The Ki-67 proliferative index was 15% of the lesional cells. No immunoreactivity was observed with synaptophysin, chromogranin, AE1/AE3, EMA, CD15, S100, AFP, CEA, HMB45, and Estrogen Receptor (Figure 4).
DISCUSSION
Pregnancy luteoma is a non-neoplastic hyperplasia of theca-lutein cells thought to be partially influenced by pregnancy hormones including human chorionic gonadotrophin (HCG). Typically, pregnancy luteoma is seen in the third–fourth decades of multiparous pregnant women. The most common presentation of luteomas include virilization, pressure symptoms due to mass effect, and hemorrhage secondary to ovarian torsion. These lesions have been reported to undergo spontaneous regression in the post-partum period [1]. The hyperplastic stromal cells secrete androgens, and the patients or infants will usually present with hyperandrogenic manifestation such as acne and hirsutism [2]. Neither our patient nor her female infant exhibited any virilization. Multiple case reports have previously described luteomas in pregnancy discovered incidentally during cesarean delivery. Our case is unique since the patient presented with a relatively large mass compared to the documented cases by Shen et al. and Dhar et al. [3],[4].
Pregnancy luteoma can be difficult to differentiate from steroid cell tumors not otherwise specified type since both have a similar histology and immunohistochemical staining profile. The factors suggestive of pregnancy luteoma include bilaterality, multifocality, and presence of follicles-like spaces with colloid-like materials. Although our case had a unilateral ovarian mass with a focal lesion, the follicles like spaces, overall histologic morphology and immunohistochemistry supported the diagnosis of pregnancy luteoma.
Short-term clinical and radiologic follow-up is recommended since the vast majority of pregnancy luteoma will regress spontaneously within three months of postpartum period [2],[5]. Although the studied cases did not have all these complications, Shen et al. described the maternal and fetal complications arising due to luteoma such as torsion of the ovarian mass and fetal adrenocortical hormone disturbance [4].
CONCLUSION
Pregnancy luteoma is a hyperplastic variant of the normal physiologic condition due to the hormonal influence during pregnancy. This is most pronounced during the third trimester although it can mimic ectopic pregnancy in the first trimester. The hyperplastic lutein cells can produce sex steroids and present with hirsutism or virilization. Most patients with pregnancy luteoma are asymptomatic and do not warrant surgical intervention even during delivery. However, close follow-up of the mother and infant is recommended to prevent any complications.
REFERENCES
1.
2.
3.
4.
5.
Khurana A, O’Boyle M. Luteoma of pregnancy. Ultrasound Q 2017;33(1):90–2. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Jennifer Lee - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jacob I Afude - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
James D Cotelingam - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Menchu Ong - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Jennifer Lee et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.